Objective: Low dose Ara-C and hypomethylating agents (HMAs) - decitabine (DEC) and azacitidine (AZA) - have made it possible to treat more elderly patients with acute myeloid leukemia (AML). Both HMAs demonstrated efficacy in monotherapy and in combination with targeted therapies. We analyzed the outcomes of elderly and unfit patients with newly diagnosed AML in our population.
Methods: Analyses of our database revealed 222 eligible AML patients from diagnosed between January 2013 to December 2020. All patients were received low intensity treatments including AZA +/- venetoclax, DEC and low dose Ara-C. The effects of cytogenetic risk group, response rate, treatment type on overall survival (OS) and PFS (progression-free survival) were evaluated. Survival analyses were performed with the Kaplan-Meier method and log-rank test. A p-value of <0.05 was considered statistically significant.
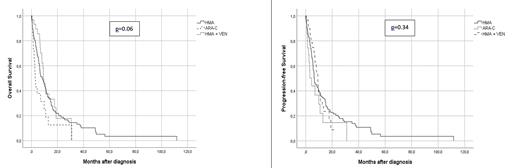
Results: Median age was 73 years (51-89). Eastern Cooperative Oncology Group (ECOG) performance score was <2 and ≥2 for 75 patients (36.8%) and 147 patients (63.2%), respectively. Of the patients 8.2% had favorable, 76.9% intermediate and 15.0% adverse risk according to European Leukemia Network (ELN) risk classification. Extramedullary involvement was present in 4.5%. Low dose treatment regimens included AZA in 119 patients (53.6%), DEC in 38 (17.6%), low dose ARA-C in 26 (11.7%) and AZA + venetoclax in 39 (17.1%). Complete remission was achieved in 61 patients (27.5%), whereas 39 patients (17.6%) had partial remission (PR) and 64 (28.8%) had stable/progressive disease (SD/PD). Overall response rate was 48.1%. CR rate was higher with AZA + venetoclax (44.7%, p=0,005) and other regimens had similar outcomes. Median OS was 10.3 months. No significant difference difference in PFS was observed between the regimens. However, the lowest PFS was observed with low-dose Ara-C (p=0.33). ELN risk groups revealed no significant effect on PFS and OS (p=0.77 and p=0.82, respectively). Infections were the most common cause of death (42.7%).
Conclusions: The prognosis of AML in the elderly remains poor. HMA monotherapy is effective among elderly and unfit patients. However, combination therapies may be more effective and safe. The incorporation of targeted therapies may provide additional benefit in this patient group. However, the accessibility of several novel targeted drugs is still very limited in many countries.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal